Understanding Bone Mineral Density Changes in Cirrhosis Patients
- Guang Chen
- Dec 17, 2025
- 3 min read
Bone health is often overlooked in patients with liver cirrhosis, yet it plays a crucial role in their overall well-being. Cirrhosis can lead to significant changes in bone mineral density (BMD), increasing the risk of fractures and complicating patient management. This article explores how cirrhosis affects bone mineral density, the mechanisms behind these changes, and practical approaches to assessment and care.
What Is Bone Mineral Density and Why It Matters
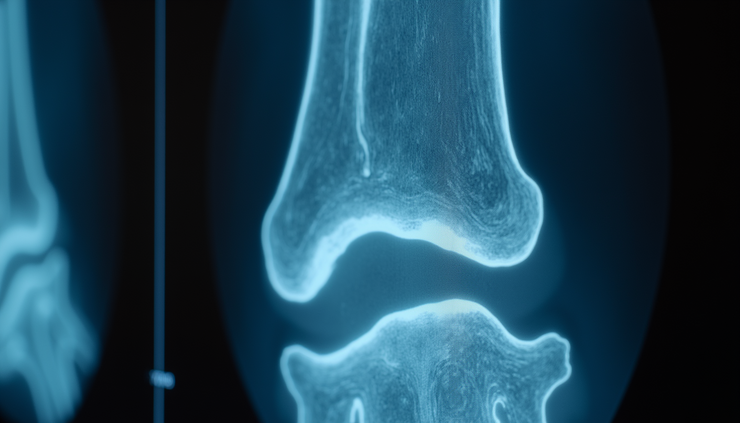
Bone mineral density measures the amount of minerals, mainly calcium, in a specific volume of bone. It reflects bone strength and helps predict fracture risk. Low BMD indicates weaker bones, which are more prone to breaks even with minor trauma.
In healthy adults, bone remodeling maintains a balance between bone formation and resorption. Disruption of this balance leads to bone loss or abnormal bone structure. For patients with cirrhosis, this balance is often disturbed, resulting in decreased BMD and increased fragility.
How Cirrhosis Affects Bone Mineral Density
Cirrhosis is the advanced scarring of the liver caused by chronic liver diseases such as hepatitis, alcohol abuse, or fatty liver disease. It affects bone health through several pathways:
Hormonal Imbalance: The liver plays a role in hormone metabolism. Cirrhosis can reduce levels of sex hormones like estrogen and testosterone, which protect bone mass.
Nutritional Deficiencies: Malabsorption and poor diet in cirrhosis patients often lead to deficiencies in calcium, vitamin D, and protein, all essential for bone health.
Inflammation and Cytokines: Chronic liver inflammation releases cytokines that stimulate bone resorption and inhibit bone formation.
Reduced Physical Activity: Fatigue and muscle weakness common in cirrhosis reduce weight-bearing activity, which is necessary to maintain bone strength.
Medications: Some drugs used in cirrhosis management, such as corticosteroids, can accelerate bone loss.
These factors combine to increase the risk of osteoporosis and fractures in cirrhosis patients.
Prevalence and Impact of Low Bone Mineral Density in Cirrhosis
Studies show that up to 70% of patients with cirrhosis have reduced bone mineral density. Osteoporosis and osteopenia are common, with fracture rates significantly higher than in the general population.
Fractures in cirrhosis patients can lead to:
Increased morbidity and prolonged hospital stays
Reduced mobility and quality of life
Higher healthcare costs
Complications in liver transplantation candidacy and recovery
Recognizing and managing bone health is therefore essential in cirrhosis care.
Assessing Bone Mineral Density in Cirrhosis Patients
Early detection of bone loss can prevent fractures and improve outcomes. The main tool for assessing BMD is dual-energy X-ray absorptiometry (DXA), which measures bone density at the spine, hip, and sometimes the forearm.
For cirrhosis patients, assessment should include:
Baseline DXA scan at diagnosis or when cirrhosis is advanced
Regular follow-up scans every 1-2 years depending on risk factors
Laboratory tests to check calcium, vitamin D, parathyroid hormone, and markers of bone turnover
Evaluation of fracture history and risk factors such as age, gender, smoking, and alcohol use
Managing Bone Health in Cirrhosis
Addressing bone mineral density changes in cirrhosis requires a comprehensive approach:
Nutritional Support
Ensure adequate intake of calcium and vitamin D
Correct malnutrition with balanced protein and calorie intake
Supplement vitamin D in cases of deficiency, guided by blood levels
Lifestyle Modifications
Encourage weight-bearing and muscle-strengthening exercises as tolerated
Advise smoking cessation and limit alcohol consumption
Prevent falls by assessing home safety and balance issues
Medical Treatments
Bisphosphonates may be used to reduce bone loss but require caution in patients with esophageal varices or renal impairment
Hormone replacement therapy can be considered in selected cases, especially postmenopausal women
Newer agents like denosumab or teriparatide may be options but need further study in cirrhosis
Monitoring and Follow-up
Regular BMD testing to track treatment response
Monitor for side effects of medications
Coordinate care between hepatologists, endocrinologists, and nutritionists
Challenges and Future Directions
Research continues to explore the best ways to prevent and treat bone loss in cirrhosis. Challenges include:
Limited data on safety and efficacy of osteoporosis drugs in advanced liver disease
Difficulty in managing nutritional deficiencies due to malabsorption
Need for better screening guidelines tailored to cirrhosis patients
Emerging therapies targeting bone metabolism and inflammation may offer new hope. Meanwhile, raising awareness among healthcare providers and patients is key.



Comments